| Category | Services |

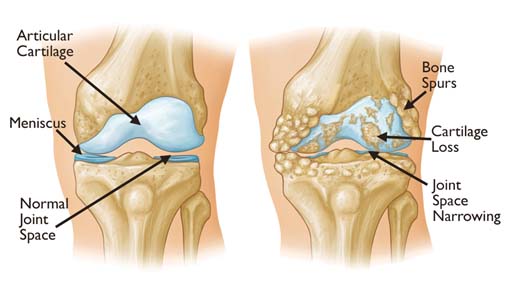

Osteoarthritis, also known as a degenerative joint disease (DJD), is the most common type of arthritis. Osteoarthritis is more likely to develop as people age. The changes in osteoarthritis usually occur slowly over many years, though there are occasional exceptions. Inflammation and injury to the joint cause bony changes, deterioration of tendons and ligaments and a breakdown of cartilage resulting in pain, swelling, and deformity of the joint.
Primary: Most common, generalized, primarily affects the fingers, thumbs, spine, hips, knees, and the great (big) toes.
Secondary: Occurs with a pre-existing joint abnormality, including injury or trauma, such as repetitive or sports-related; inflammatory arthritis, such as rheumatoid, psoriatic, or gout; infectious arthritis; genetic joint disorders, such as Ehlers-Danlos (also known as hypermobility or "double-jointed; congenital joint disorders; or metabolic joint disorders.
Approximately 80% of older adults, ages 55 years and older, have evidence of osteoarthritis on X-ray. Of these, an estimated 60% experience symptoms. Post-menopausal women have an increased incidence of knee osteoarthritis compared to men.
In addition to age and secondary causes such as inflammatory arthritis and prior injury/ trauma, several other risk factors increase the chance of developing osteoarthritis including obesity, diabetes, elevated cholesterol, sex, and genetics.
Obesity is a risk factor for osteoarthritis, particularly of the knee. In addition to overloading the weight-bearing mechanisms of the body, the metabolic and pro-inflammatory effects of obesity have been studied as contributory to osteoarthritis. Maintaining ideal body weight or losing extra weight is important for those at risk.
Both diabetes and hyperlipidemia (elevated lipids/cholesterol) contribute to the inflammatory response within the body, increasing the risk of osteoarthritis.
Heredity can play a role in osteoarthritis, as individuals born with other bone diseases or genetic traits may be more likely to develop osteoarthritis. For example, Ehlers-Danlos, which is characterized by joint laxity or hypermobility, can contribute to osteoarthritis.
There is no cure for osteoarthritis. Mild to moderate symptoms are usually well managed by a combination of pharmacologic and non-pharmacologic treatments. Medical treatments and recommendations include:
Decrease joint pain and stiffness and delay further progression.
Improve mobility and function.
Increase patients' quality of life.
The type of treatment regimen prescribed depends on many factors, including the patient's age, overall health, activities, occupation, and severity of the condition.
Medications (topical pain medicines and oral analgesics including nonsteroidal anti-inflammatory medications, NSAIDs).
Physical and occupational therapy.
Weight loss (if overweight).
Healthy eating, managing diabetes and cholesterol.
Supportive devices such as braces, orthotics, shoe inserts, cane, or walker.
Intra-articular injection therapies (steroid, hyaluronic acid “gel”, PRP).

Platelet-rich plasma is a form of regenerative medicine. It uses injections of your own blood platelets to help with healing.
Platelets, or thrombocytes, are a type of blood cell. Their main function is clotting blood. They’re produced in your bone marrow. Platelets contain growth factors. These are proteins that may be helpful in healing injuries.
A healthcare professional will collect a small amount of your blood (approx. 15-20 ml only). They will place your blood into a centrifuge. This spins your blood at different speeds until it separates into different layers. One layer is the platelet-rich plasma. This layer of plasma may have as much as three-four times more platelets than regular blood.
The platelet-rich plasma will then be injected into your affected area. We will first numb the area with a local anaesthetic. The pain at the site may increase for the first 1-2 days. It could take 1 week before you feel any improvement.
Avoid taking non-steroidal anti-inflammatory medications ( NSAIDs) after your treatment as this may block the effect
Avoid activities that put stress on the area of treatment for a few days
The effectiveness of platelet-rich plasma treatment depends on several factors, including:
Your overall health
Whether your injury is chronic (it developed over time) or acute (sudden and serious)
Which part of your body needs treatment
The preparation of the platelet-rich plasma treatment
Many clinical trials have supported its use.
Studies have shown that platelet-rich plasma treatment is effective in improving low-to moderate-grade knee osteoarthritis.
Some studies have found that platelet-rich plasma injections significantly reduced pain compared to placebos. People’s physical function also improved significantly. These benefits continued at 3, 6 and 12-month follow-ups.
There’s no chance of an allergy or immune reaction to platelet-rich plasma treatment because the plasma is taken from your own blood. Side effects and complications are rare
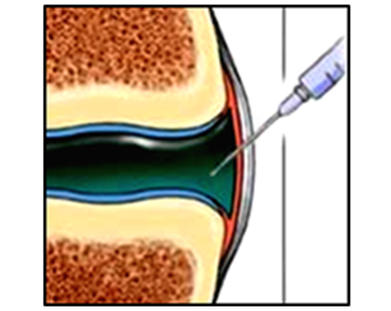
The doctor will clean the area over the joint and insert a small needle into the fluid filled area around the joint bones under imaging guidance. When it is in the correct position, they will inject the PRP into the joint. They will remove the needle and cover the injection site with a small dressing.
Occasionally it is difficult to inject much medicine into the joint space, especially if the joint is extremely swollen. If this is the case, other medicines may be prescribed to reduce the swelling before the injections are tried again.
We have very fast and competent working team (Consultant, fellow, clinical assistant, technician and ward assistant) which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around few hours.
Every procedure carries a risk, although this is extremely small. The risk of infection with this procedure is extremely small as no incisions are made in the skin.
You can resume your work after 1 day if existing disease allows.

Rheumatoid arthritis (RA) is a chronic autoimmune and inflammatory disease that causes pain, swelling, and stiffness in the joints. It affects the small joints like hands and feet and causes bone erosion and joint deformity.
It occurs when your immune system mistakenly attacks your own body's tissues. Unlike the wear-and-tear damage of osteoarthritis, rheumatoid arthritis affects the lining of your joints, causing a painful swelling that can eventually result in bone erosion and joint deformity.
The immune cells attack the joint lining leading to inflammation and periods of flare or exacerbations. It is during these periods that most of the clinical signs and symptoms appear. The symptoms in RA are as follows
RA affects the smaller joints of the hand and feet first and then progresses to the hips, knees, ankles, elbows, and wrists.
Rheumatoid arthritis is diagnosed based on signs and symptoms, medical history, physical examination, and diagnostic tests.
Many tests are performed to confirm the diagnosis of rheumatoid arthritis. These tests are
Imaging tests like X-rays, MRI, and ultrasound are also performed to judge disease severity.
Fortunately, clinical studies report disease remission in patients who adhere to the treatment. Depending on disease severity, the following drugs may be recommended,
If medications and therapies don’t work, surgeries may become necessary to repair damaged joints. Surgery may involve the following procedures
Ultrasonography-guided intraarticular steroid injection is one of the important treatments for Rheumatoid arthritis.
Intra-articular steroid injection
It is an injection of steroid inside the synovial cavity of the joint or around the joint capsule
The most common type of steroids that are used for intraarticular use are Methyl Prednisolone and Triamcinolone. Besides, depo preparation of Dexamethasone and Betamethasone are also available and used occasionally.
Depo-preparation of steroids do not have many systemic effects when injected within joints and used within recommended doses. These depo-preparation are particulate steroids having prolonged effects for several weeks and that’s why they should not be repeated too often particularly within one month. Actually, repeated use of depot steroids can have cumulative effects and might have more side effects.
Thus, an intraarticular steroid is safe if used within recommended doses and if not repeated within one month.
The dose of steroids depends on the size of the joint. Thus, 5-40 mg of depo methylprednisolone or equivalent dose is used for small joints like facet joints, Sacroiliac joints, wrist joints, interphalangeal joints. Whereas, 20-80 mg of depo methylprednisolone or equivalent dose is used for large joints like knee joint, hip joint, shoulder joint, etc.
Earlier, the injection of steroids was done in blind and landmark techniques. Thus, chances of inappropriate injection were a possibility. So, to minimize the possibility of inaccurate injection of steroids, larger doses and volumes were used so that some amount is installed inside the joint or at least around the joint.
Nowadays it is recommended to inject every intraarticular injection under imaging guidance like C-arm or ultrasonography. So, with real-time image physician can see the needle tip inside the joint and inject it in the proper position.
Thus, with accurate placement of the needle, success can be assured and the total doses of steroids can be minimized.
There are several indications of intraarticular steroid injections. These are:
The most common indication is inflammation of joints in rheumatoid arthritis or spondylo-arthritis. Commonly injected joints are wrist joints, interphalangeal joints, knee joints, hip joints, shoulder joints, ankle joints, facet joints, sacroiliac joints, etc.
It is also indicated in degenerated arthropathies particularly when it is associated with joint effusion. However, regeneration therapies with platelet rich plasma, bone marrow aspirate, or adipose tissues are better choices for degenerated joints which is more commonly known as osteoarthritis.
Sometimes it is used in crystal arthropathies like pseudogout.
There are several indications of steroid use other than joints. The indications are:
Sometimes depo methylprednisolone is used in systemic inflammatory conditions like rheumatoid arthritis flare-up, or in spondyloarthropathies.
The doctor will clean the area over the joint and insert a small needle into the fluid filled area around the joint bones under imaging guidance. When it is in the correct position, they will inject a mixture of steroid medicine and local anaesthetic. They will remove the needle and cover the injection site with a small dressing
Occasionally it is difficult to inject much medicine into the joint space, especially if the joint is extremely swollen. If this is the case, other medicines may be prescribed to reduce the swelling before the injections are tried again.
We have a very fast and competent working team (Consultant, fellow, clinical assistant, technician and ward assistant) which provides you a comfortable atmosphere and eases your nerves. The usual time of stay is around few hours.
Every anaesthetic carries a risk, although this is extremely small. The risk of infection with this procedure is extremely small as no incisions are made in the skin.
You can resume your work after 1 day if existing disease allows.